Learn about Jennifer Hernandez' path through nursing school and how her clinical experiences inspired her…


Apr 15, 2024 | Career Insights, Nursing
Today’s nurses do it all: offer clinical care, maintain sanitary environments, and provide comfort for patients as they face distressing circumstances. They must accomplish all this while abiding by evidence-based practices and keeping up to date on quickly...
Apr 14, 2024 | Nursing
There are countless stories of courageous and inspiring nurses that continue to influence nursing practice today. We honor 26 of them here!

Apr 12, 2024 | Nursing, Program Insights
When you already have the education, licensing, and training needed to become a registered nurse (RN), you might want to enhance your skills as you consider different nursing career paths. As an RN, you already have an advantage in terms of training and education...
Mar 29, 2024 | Nursing, Program Insights
Should you aim to become a nurse leader or nurse manager? Learn more about the differences between these roles in the nursing field.

Mar 25, 2024 | Career Insights, Nursing
At a time when hospitals and medical centers are struggling to adequately staff their nursing departments, nursing schools across the United States are regularly turning qualified applicants away due to a lack of dedicated faculty members. In its attempts to raise...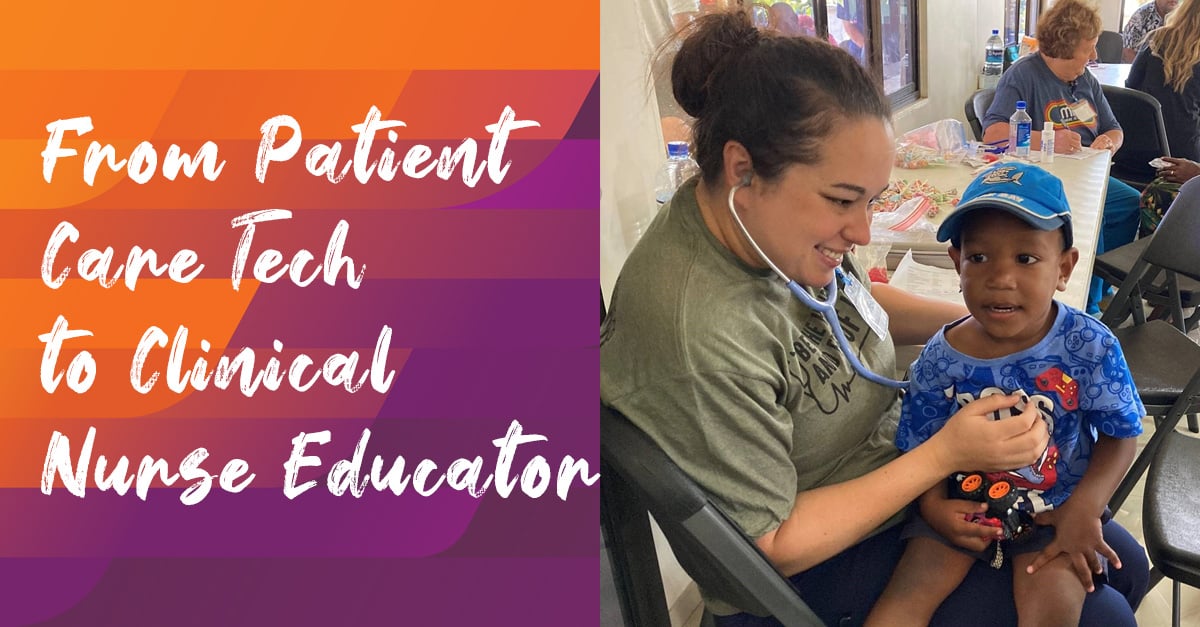
Mar 22, 2024 | Nursing, Student Spotlights
As a high school student in Georgia, Halea Caudill participated in a dual enrollment pathway to earn her Certified Nurse Aide credential while pursuing her high school diploma. “That’s when I realized how much I enjoyed patient care and that nursing was my ultimate...
Learn about Jennifer Hernandez' path through nursing school and how her clinical experiences inspired her…
Tom Cualing knew right away he wanted to follow in his father's footsteps by entering…
Brittane Strahan's parents worked in different areas of a hospital, and this allowed her to…